Hospital pharmacy is a specialized field within the practice of pharmacy that functions within hospitals or healthcare facilities. In contrast to community pharmacies, hospital pharmacies work closely with medical staff to ensure the highest quality of patient care. The primary objective is to manage the medication needs of inpatients and occasionally outpatients, with an emphasis on safe, effective, and cost-efficient drug therapy.
What is a Hospital Pharmacy?
A hospital pharmacy is an essential department within a hospital that focuses on the procurement, storage, preparation, dispensing, and monitoring of medications. Its primary role is to ensure patient safety and enhance therapeutic outcomes. By managing these processes, the hospital pharmacy significantly contributes to patient care and medication management within the healthcare setting.
Core Functions of a Hospital Pharmacy
1. Medication Procurement and Inventory Management
Hospital pharmacists work quietly behind the scenes to make sure the right medications are always on hand when patients need them most. They take great care in everything from buying the medicines to storing them properly, making sure each one stays safe, effective, and ready to use.
These pharmacists also work closely with suppliers to maintain optimal stock levels, avoiding both waste from over-ordering and problems from running out of essential medicines. Their attention to detail helps the entire hospital run smoothly and keeps patient care on track.
2. Prescription Dispensing
Hospital pharmacists take great care in filling prescriptions, mainly for patients staying in the hospital and sometimes for those heading home.
They double-check every detail to make sure the medication is accurate, calculate the right dose tailored to each patient, and cross-reference with medical histories to avoid any mistakes.
This careful attention helps keep patients safe and makes their recovery as smooth as possible.
3. Clinical Pharmacy Services
In hospitals, pharmacists are not merely individuals behind the counter; they are valued members of the healthcare team who are genuinely dedicated to each patient’s well-being.
They apply their extensive knowledge to understand the mechanisms of medications, monitor for potential side effects, and ensure that drug combinations are both safe and effective.
By collaborating closely with doctors and nurses, pharmacists play a crucial role in making informed treatment decisions.
4. Medication Therapy Management (MTM)
Medication Therapy Management is all about taking a broader view. Hospital pharmacists take the time to review everything a patient is taking—from prescription drugs to over-the-counter medications—to ensure that treatments are working well together.
By doing this, they help improve health outcomes, avoid unnecessary or duplicate medications, and reduce the risk of harmful side effects. It’s a thoughtful and personalized approach that prioritizes patient safety.
5. Sterile and Non-Sterile Compounding.
Hospital pharmacies play a crucial role in patient care by preparing medications tailored to each person’s unique needs. This might include custom IV solutions, carefully measured chemotherapy drugs, or special doses for children.
These aren’t off-the-shelf medications—they’re made with precision and care. To ensure everything is safe and effective, pharmacists follow strict sterile (aseptic) procedures at every step of the preparation process. It’s detailed, delicate work that directly supports better outcomes for some of the most vulnerable patients.
The Role of the Hospital Pharmacist
Hospital pharmacists are experts who play an important role in keeping patients healthy. With their specialized training, they work hard to ensure that everyone gets the right medication for their unique needs. They’re dedicated to connecting medication management with patient well-being, making sure each person receives the personalized care they deserve! This approach ensures that the treatment is both safe and effective, tailored to meet the individual needs of each patient.
Their responsibilities include:
- Evaluating medication orders
- Consulting with physicians and nurses
- Monitoring therapeutic drug levels
- Educating patients during discharge
- Participating in clinical trials and research
Difference Between Hospital Pharmacy and Community Pharmacy
Hospital pharmacies and community pharmacies may both deal with medications, but their day-to-day work and environments are quite different. Hospital pharmacies are located right inside hospitals or healthcare centers, focusing mainly on the needs of patients who are admitted. Hospital pharmacists are an important part of the medical team—they work closely with doctors, nurses, and other healthcare professionals, ensuring patients get the best possible care.
Their work often involves preparing sterile medicines, managing complex treatment plans, and carefully monitoring drug levels to keep everything safe and effective. They handle some of the most specialized and high-risk medications, like chemotherapy drugs and IV antibiotics, playing a crucial role in helping patients through some of their toughest health challenges.
On the other hand,
Community pharmacies are usually found in places like drugstores or supermarkets, serving people from all walks of life. Community pharmacists are often the friendly faces patients see when picking up their prescriptions or buying over-the-counter medicines. Beyond just dispensing meds, they’re there to offer advice, answer questions, and help people manage long-term conditions like diabetes, asthma, or high blood pressure. They keep the community healthy by providing services like vaccinations and wellness tips. While their role in clinical decisions is more limited compared to hospital pharmacists, their day-to-day support makes a big difference in people’s lives.
In summary, hospital pharmacies concentrate on inpatient care and clinical collaboration, whereas community pharmacies prioritize accessibility, direct patient service, and routine medication dispensing. Both types of pharmacies are essential components of the healthcare system, operating in different environments and fulfilling distinct roles.
Importance of Hospital Pharmacy in Healthcare
Hospital pharmacies are integral to the overall effectiveness of modern healthcare systems, influencing patient outcomes in several profound ways:
- Reducing medication errors
- Ensuring timely drug administration
- Supporting antimicrobial stewardship
- Improving patient recovery rates
- Promoting cost-effective treatments

1. Reducing Medication Errors:
By meticulously overseeing the procurement, storage, and dispensation of medications, hospital pharmacies significantly diminish the likelihood of medication errors, making sure that patients receive the correct drugs in the appropriate dosages.
2. Ensuring Timely Drug Administration:
Hospital pharmacists play a crucial role in coordinating and managing medication schedules and facilitating timely drug administration, which is pivotal for achieving optimal therapeutic outcomes.
3. Supporting Antimicrobial Stewardship:
Through vigilant monitoring and management of antimicrobial therapies, hospital pharmacies play a crucial role in combating antibiotic resistance, promoting the responsible use of these critical medications while ensuring their efficacy.
4. Improving Patient Recovery Rates:
By providing expert guidance on medication management and side effect mitigation, hospital pharmacies help expedite patient recovery, enabling individuals to transition from hospital care to home more smoothly and safely.
5. Promoting Cost-Effective Treatments:
Through comprehensive assessments of medication treatments and suggesting economical alternatives, hospital pharmacies improve patient care. It also plays a significant role in the financial sustainability of healthcare organizations.
Challenges Faced by Hospital Pharmacies
Though hospital pharmacies play a vital role in patient care, they face numerous significant challenges that can impact their effectiveness:
Rising drug costs
One of the most pressing issues is the rising cost of medications, which strains budgets and complicates the procurement process. As pharmaceutical prices continue to skyrocket, hospitals are faced with the crucial challenge of balancing the imperative to deliver top-notch patient care with the pressing need to manage financial limitations.
Shortage of skilled pharmacists
There is a notable shortage of skilled pharmacists, which exacerbates existing workload pressures. This scarcity can lead to increased stress for pharmacy staff, potentially compromising the quality of service delivered to patients.

Regulatory compliance
Regulatory compliance is another formidable challenge. Hospital pharmacies must adhere to stringent and ever-changing regulations, which require continuous education and can divert resources from patient-focused activities.
Inventory shortages
Moreover, inventory shortages pose a considerable risk to patient safety and treatment efficacy. Supply chain disruptions can result in critical medications being unavailable, forcing pharmacists to seek alternatives that may not be as effective.
Increasing demand for personalized medicine
Finally, the growing demand for personalized medicine adds complexity to the operations of pharmacies. As therapies become more tailored to individual patients, hospital pharmacies must adapt quickly to accommodate specialized treatments, all while ensuring they have the necessary resources and expertise.
Collectively, these challenges underscore the essential need for innovative solutions and support within hospital pharmacies.
Future Trends in Hospital Pharmacy
The field of hospital pharmacy is experiencing significant evolution. Key trends include:
1. Automation and Robotics
Automated dispensing systems are revolutionizing medication management by streamlining the dispensing process, which significantly enhances efficiency while effectively minimizes the risk of human error.
These advanced systems ensure precise dosages, improve inventory management, and contribute to a safer pharmaceutical environment within healthcare facilities.
2. Telepharmacy
Telepharmacy is breaking down geographical barriers by providing remote access to clinical pharmacists, thereby improving healthcare accessibility for patients in rural and underserved communities.
This groundbreaking approach empowers patients to access expert care and guidance without the challenges of travel, ensuring that even those in the most remote areas can benefit from professional medication management and consultation.
3. Pharmacogenomics
The exciting fusion of pharmacogenomics into the world of clinical practice is gaining considerable momentum in hospital settings, where the application of genetic information enables the tailoring of drug therapy to personalized patient care.
This approach not only enhances treatment efficacy but also helps minimize adverse effects by ensuring that medications are selected based on a patient’s unique genetic profile.
4. Artificial Intelligence in Drug Management
Artificial intelligence is quickly becoming a valuable ally in how hospitals manage medications. These smart tools help healthcare professionals spot potential drug interactions, fine-tune dosages, and keep an eye out for harmful side effects—often before they happen.
By tapping into huge amounts of data, AI supports better, faster decision-making at the bedside. The result? Safer treatments and better outcomes for patients.
How to Become a Hospital Pharmacist
To be a hospital pharmacist, individuals generally need to fulfill several key educational and professional requirements:
1. Educational Qualifications:
A Bachelor of Pharmacy (BPharm) or Doctor of Pharmacy (PharmD) degree from an accredited institution is essential. The PharmD program typically includes extensive coursework in pharmacology, medicinal chemistry, and therapeutics, as well as hands-on clinical training.
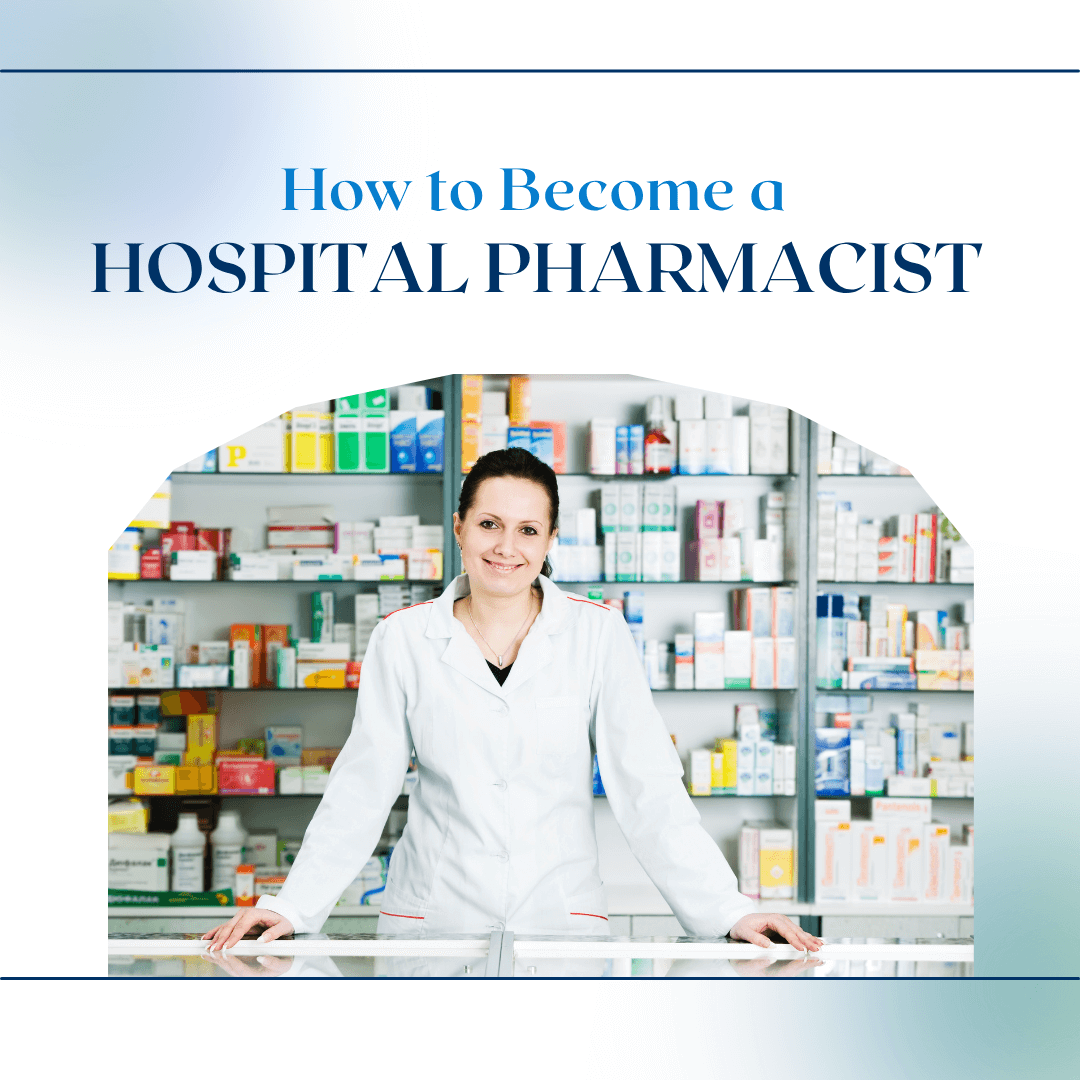
2. Licensing:
After completing the degree, aspiring pharmacists must obtain a license from the relevant pharmacy council or board in their region.
This process typically involves passing a national or state examination, such as the North American Pharmacist Licensure Examination (NAPLEX) in the United States.
Candidates may also need to pass a jurisprudence exam that assesses their knowledge of state-specific pharmacy laws.
3. Clinical Internship:
Gaining real-world experience through a clinical internship or hospital training is an essential part of becoming a hospital pharmacist.
It’s during this time that students move beyond textbooks and step into the heart of patient care. They get hands-on experience managing medications, working directly with patients, and collaborating with doctors, nurses, and other healthcare professionals.
This training builds confidence and helps future pharmacists understand how to improve treatment outcomes.
4. Specialization (Optional):
While not mandatory, pursuing additional specialization can enhance career prospects. Areas of focus may include oncology, pediatrics, geriatrics, or critical care.
Specialized training programs or residencies typically require further education and can significantly elevate a pharmacist’s expertise and employability within specific hospital departments.
In conclusion, Hospital pharmacies are truly at the heart of delivering safe, effective, and evidence-based care. As healthcare becomes more centered around individual patients and driven by technology, hospital pharmacists are taking on bigger, more dynamic roles.
They’re no longer just handling medications—they’re part of the care team, helping plan treatments, making critical decisions, and ensuring every patient gets the right therapy at the right time.
With their growing responsibilities and specialized knowledge, hospital pharmacists are shaping a future where patient care is smarter, safer, and more personalized than ever before.
FAQ
Q1: What is the difference between clinical pharmacy and hospital pharmacy?
A: Clinical pharmacy is a branch within hospital pharmacy that focuses on direct patient care and drug therapy optimization.
Q2: Do hospital pharmacies serve outpatients?
A: Some hospital pharmacies serve outpatients, especially during discharge or follow-up care.
Q3: Can hospital pharmacists prescribe medications?
A: In some countries or under specific collaborative agreements, hospital pharmacists can adjust or prescribe medications.
Q4: What is sterile compounding?
A: It refers to the preparation of medication in a sterile environment, often used for injectables, eye drops, or chemotherapy.